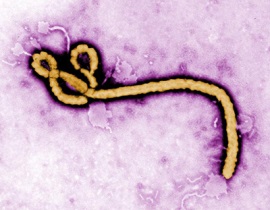
by Brianna Crandall — October 20, 2014—Many facilities managers who have been listening to the news in recent weeks have understandable concerns about the possibility of the Ebola virus making its way to their facilities, particularly if they work in health care or an industry related to travel services here in the United States, or if they live in or near an area with an outbreak of the life-threatening disease.
In response to widespread concerns, several government agencies and other organizations have been publishing the current research on what Ebola is, how it spreads, and how infection can be prevented. Since FMs play an important role in keeping facilities clean and equipment sanitized in order to help prevent the spread of any infectious disease, FMLink has gathered and presented below several of the most relevant resources.
FMLink recommends that our readers educate themselves about the disease from some of the resources listed below, train their staff, and set up emergency and contingency plans in case of an outbreak of any kind. Suggested preparations could include having a room available in which employees or others can remain in isolation until trained medical staff arrives, keeping in stock sufficient supplies of appropriate disinfectant products, and preparing for how work duties will be performed if several of the staff are ill.
Who is at risk
As heard daily in the news, Ebola viruses are capable of causing severe, life-threatening disease, called Ebola hemorrhagic fever (EHF). Although only a few cases have been confirmed in the United States (see CNN’s “Ebola in U.S.: Who has it, who doesn’t, who might,” updated October 17, for a list), workers performing tasks involving close contact with symptomatic individuals with EHF or in environments contaminated or reasonably anticipated to be contaminated with infectious body fluids are potentially at risk of exposure.
This may include workers in the health care, mortuary and death care, airline, and other travel service industries. Workers who interact with people, animals, goods, and equipment arriving in the United States from foreign countries with current EHF outbreaks are at the greatest risk for exposure. See the U.S. Centers for Disease Control and Prevention’s (CDC)’s National Institute for Occupational Safety and Health’s (NIOSH) Ebola page for the latest news about outbreaks, transmission, risk of exposure, prevention and more.
Transmission
According to the World Health Organization’s (WHO) Ebola virus disease and Frequently asked questions on Ebola virus disease Web pages , fruit bats (Pteropodidae) are considered the likely host of the Ebola virus, which affects both humans and primates, but in the current outbreak in West Africa, the majority of cases in humans have occurred as a result of human-to-human transmission.
According to WHO, infection occurs from direct contact through broken skin or mucous membranes with the blood, or other bodily fluids or secretions (stool, urine, saliva, semen) of infected people, including those who have died. Infection can also occur if broken skin or mucous membranes of a healthy person come into contact with environments that have become contaminated with an Ebola patient’s infectious fluids such as soiled clothing, bed linen, or used needles.
Symptoms and what to do
CDC’s Advice for Humanitarian Aid Workers Traveling to Guinea, Liberia, or Sierra Leone during the Ebola Outbreak Web page recommends that a person who may have potentially been exposed to Ebola within the last 21 days should seek medical care immediately if they develop fever (100.4°F / 38°C or higher) or other symptoms such as severe headache, muscle pain, vomiting, diarrhea, stomach pain, or unexplained bleeding or bruising. Persons exposed to the Ebola virus are not contagious until they display symptoms themselves, according to CDC.
CDC advises the person to notify their organization that they have become ill, and to give advance notice to the doctor about their symptoms prior to going to the doctor’s office or hospital. CDC also says the person should limit their contact with other people when they travel to the doctor, and to avoid public transportation. The person should not travel anywhere except to the doctor’s office or hospital.
Extrapolating for facilities managers and other employers, workers should be trained to recognize these symptoms in themselves and others. Anyone displaying these symptoms, particularly a fever, who thinks they may have been exposed to Ebola in the last 21 days, should be immediately isolated, and note taken of who they have been in contact with. The person should seek medical attention as soon as possible, but avoid public transportation—preferably waiting until trained medical personnel can arrive.
Prevention
The U.S. Occupational Safety and Health Administration (OSHA) published a new Ebola Safety and Health Topics Web page that provides information about the Ebola virus, including: Background, including the origins of Ebola virus and EHF; Hazard recognition; Medical information; Standards for protecting workers from Ebola virus; Control and prevention of EHF; and Additional resources.
According to OSHA, precautionary measures for preventing exposure to the Ebola virus depend on the type of work, potential for Ebola-virus contamination of the work environment, and what is known about other potential exposure hazards. OSHA notes that infection control strategies may have to be modified to include additional selections of personal protective equipment (PPE), administrative controls, and/or safe work practices.
OSHA’s Control and Prevention page outlines OSHA’s interim guidance to help prevent at-risk worker exposure to Ebola virus and individuals with EHF.
OSHA’s more general Protecting Workers during a Pandemic publication advises employers to train all workers on these basic principles of worker protection:
- Consistently practice social distancing.
- Cover coughs and sneezes.
- Maintain hand hygiene.
- Clean surfaces frequently.
The document says that employers should select equipment, such as surgical masks and respirators, that will protect workers against infectious diseases to which they may be exposed. It also suggests that employers may need to modify the work environment and/or change work practices to provide additional protection to workers and clients. For example, employers may:
- Install physical barriers (e.g., clear plastic sneeze guards);
- Conduct business in a different manner (e.g., use drive-through service windows, implement telework arrangements);
- Improve ventilation (e.g., install high-efficiency air filters, increase ventilation rates);
- Install additional hand sanitizer dispensers;
- Provide facial tissues; and
- Have workers use PPE.
Cleaning and disinfection
OSHA’s Cleaning and Decontamination of Ebola on Surfaces fact sheet provides guidance on protecting workers in non-healthcare and non-laboratory settings from exposure to Ebola, and from harmful levels of chemicals used for cleaning and disinfection. The document offers specific guidelines for facilities and janitorial staff. A sample of OSHA’s guidelines for cleaning and disinfection follows:
- Immediately clean and disinfect any visible surface contamination from blood, urine, feces, vomit, or other body fluids that may contain Ebola virus.
- Isolate areas of suspected Ebola virus contamination until decontamination is completed to minimize exposure to individuals not performing the work.
- Cover spills with absorbent material (e.g., paper towels), then pour disinfectant on to saturate the area, and allow bleach to soak into spills for at least 30 minutes before cleaning to allow it to kill any virus or other infectious agents that may be present.
- Treat any visible contamination or bulk spill matter with a suitable disinfectant (described on p. 2) before cleaning up and removing bulk material.
- After disinfecting and removing bulk material, clean and decontaminate the surface using the disinfectant.
- Ensure adequate ventilation in areas where workers are using disinfectants, including by opening windows and doors, or using mechanical ventilation equipment.
- In some cases, the use of chemical disinfectants may require an employer to train workers about how to protect themselves against chemical hazards and comply with OSHA’s Hazard Communication, 29 CFR 1910.1200, and other standards.
- Use tools, such as tongs from a spill kit, as much as possible rather than doing cleanup work directly with gloved hands.
- After cleaning and disinfection work is complete, remove PPE as follows: gloves, face shield/goggles, gown, and then mask/respirator. Wash hands with soap and water, or use an alcohol-based hand gel if no running water is available. See CDC fact sheet on donning and removal of PPE.
- Avoid cleaning techniques, such as using pressurized air or water sprays, that may result in the generation of bio-aerosols (aerosolized droplets containing infectious particles that can be inhaled).
OSHA’s Additional Resources page also has links to several documents with guidelines for specific worker populations, such as healthcare workers, airline cabin crews, mortuary and death care workers, laboratory workers, emergency responders and other at-risk professionals.
Assistance for employers
For employers with questions or concerns about Ebola, OSHA’s On-site Consultation Program offers free and confidential advice to small and medium-sized businesses in all states across the country, with priority given to high-hazard worksites. On-site Consultation services are separate from enforcement and do not result in penalties or citations, notes OSHA. Consultants from state agencies or universities work with employers to identify workplace hazards, provide advice on compliance with OSHA standards, and assist in establishing safety and health management systems. To locate the nearest OSHA On-site Consultation Program, call 800/321-OSHA (6742) or visit OSHA’s On-site Consultation Web page.





